Definition and Classification
Erectile dysfunction (ED) is the persistent inability to attain and maintain an erection sufficient for satisfactory sexual performance. It impacts psychosocial health and quality of life for both patients and partners. ED is commonly classified as organic, psychogenic, or mixed, though most cases have mixed etiology—use "primary organic" or "primary psychogenic" for clarity.
Risk factors
Erectile dysfunction (ED) is a multifactorial condition caused by vascular, hormonal, neurological, and psychological factors. It is commonly associated with aging, diabetes, hypertension, heart disease, obesity, smoking, sedentary lifestyle, and certain medications. ED is also linked to mental health conditions, chronic illnesses, sleep disorders, and may occur after COVID-19 infection. Additionally, ED is often associated with other urological conditions such as prostate disorders, urinary symptoms, chronic pelvic pain, and premature ejaculation.
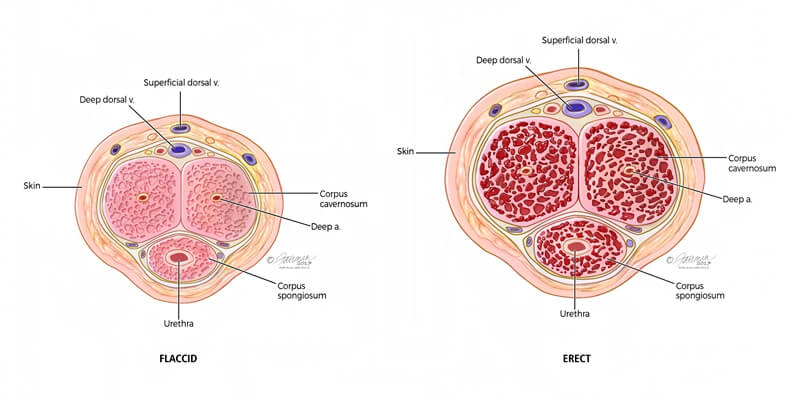
Pathophysiology
The pathophysiology of erectile dysfunction may be vasculogenic, neurogenic, anatomical, hormonal, drug-induced, or psychogenic. In most cases, multiple factors coexist and together impair erectile function.
Pathophysiology of Erectile Dysfunction (ED)
| Category | Causes / Conditions |
|---|---|
| Vasculogenic | Cigarette smoking, lack of physical exercise, obesity, cardiovascular diseases (hypertension, coronary artery disease, peripheral vascular disease), diabetes mellitus (Type 1 & 2), hyperlipidaemia, metabolic syndrome, hyperhomocysteinemia, major pelvic surgery, pelvic or retroperitoneal radiotherapy |
| Neurogenic – Central Causes | Degenerative disorders (multiple sclerosis, Parkinson’s disease, multiple system atrophy), spinal cord trauma or disease, stroke, central nervous system tumors |
| Neurogenic – Peripheral Causes | Diabetes mellitus (Type 1 & 2), chronic renal failure, chronic liver failure, polyneuropathy, major pelvic or retroperitoneal surgery or radiotherapy, urethral surgery |
| Anatomical / Structural | Hypospadias, epispadias, micropenis, phimosis, Peyronie’s disease, penile cancer and other external genital tumors |
| Hormonal | Diabetes mellitus, metabolic syndrome, hypogonadism, hyperthyroidism, hyper- or hypocortisolism, panhypopituitarism, multiple endocrine disorders |
| Mixed Pathophysiological Pathways | Chronic systemic diseases (diabetes, hypertension, metabolic syndrome, chronic kidney or liver disease, COPD, rheumatic disease), psoriasis, gouty arthritis, ankylosing spondylitis, non-alcoholic fatty liver disease, chronic periodontitis, open-angle glaucoma, inflammatory bowel disease, chronic fatigue syndrome, allergic rhinitis, obstructive sleep apnoea, depression |
| Iatrogenic Causes | Medical procedures such as TRUS-guided prostate biopsy |
| Drug-Induced | Antihypertensives (thiazide diuretics, beta-blockers), antidepressants (SSRIs, tricyclics), antipsychotics, antiandrogens (GnRH analogues or antagonists, 5-ARIs), recreational drugs, excessive alcohol intake |
| Psychogenic | Generalized type (reduced arousability, intimacy disorders), situational type (partner-related or performance-related issues, psychological distress) |
| Trauma | Penile fracture, pelvic fracture |
Pelvic surgery and prostate cancer treatment
Pelvic surgery, particularly for prostate, bladder, and colorectal cancers, can negatively affect erectile function by damaging the neurovascular bundles involved in erection, even though nerve-sparing techniques are widely used. Among pelvic cancers, prostate cancer has the strongest evidence linking treatment to erectile dysfunction. Both surgical and non-surgical treatments, including radiotherapy and brachytherapy, are associated with reduced erectile function.
Studies show a significant decline in erectile function over time after prostate cancer treatment, with the lowest recovery rates seen after radical prostatectomy. Post-surgical erectile dysfunction affects a large proportion of patients, while spontaneous recovery occurs in only a minority. Age, baseline erectile function, and surgical expertise are key factors influencing recovery.
Erectile dysfunction is also common after radiation-based therapies, with prevalence increasing over long-term follow-up. Newer focal and minimally invasive treatments appear to have a lower impact on erectile function, with many patients regaining function within one year.
Summary of evidence on the epidemiology/aetiology/pathophysiology of ED
Summary of Evidence
| Evidence Statement | LE |
|---|---|
| Erectile dysfunction is common worldwide. | 2b |
| Erectile dysfunction shares common risk factors with cardiovascular disease. | 2b |
| Lifestyle modification, including regular exercise and reduction in BMI, can improve erectile function. | 1b |
| Erectile dysfunction is a symptom rather than a disease, and underlying conditions may go undiagnosed or untreated without proper evaluation. | 4 |
| Erectile dysfunction is common after radical prostatectomy, irrespective of the surgical technique used. | 2b |
| Erectile dysfunction is common after external radiotherapy and brachytherapy. | 2b |
| Erectile dysfunction is less common after cryotherapy and high-intensity focused ultrasound. | 2b |
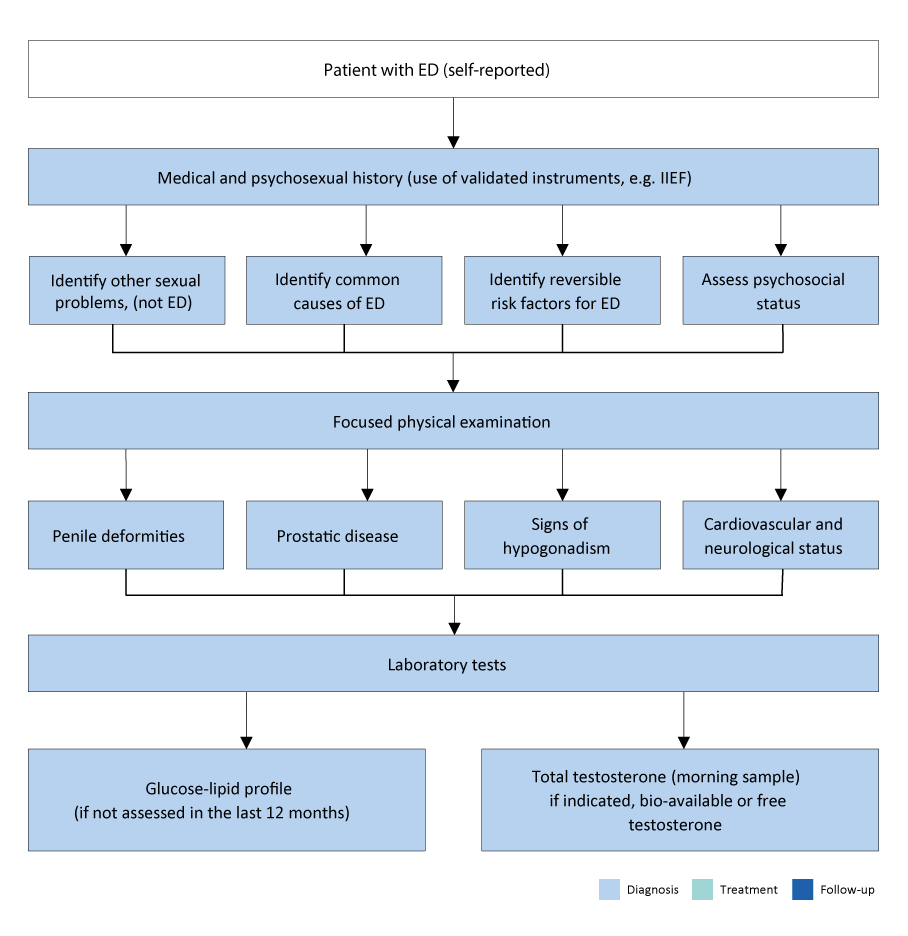
Diagnostic evaluation (basic work-up)
Medical and sexual history
The evaluation of erectile dysfunction begins with a detailed medical and sexual history of the patient and, when possible, their partner. Assessment should include the rigidity and duration of erections (both spontaneous and sexually stimulated), as well as issues related to sexual desire, arousal, ejaculation, and orgasm.
Validated tools such as the IIEF or SHIM questionnaires and the Erectile Hardness Score help assess erectile function and treatment impact. Patients should also be screened for symptoms of hypogonadism, including reduced libido, low energy, and fatigue.
Physical examination
All patients should undergo a focused physical examination of the genitourinary, endocrine, vascular, and neurological systems. This examination may identify conditions such as Peyronie’s disease, genital lesions, prostate abnormalities, or signs of hypogonadism.
Blood pressure, heart rate, and body measurements such as BMI or waist circumference should also be assessed to evaluate cardiovascular and metabolic risk factors.
Laboratory testing
Patients should undergo fasting blood glucose or HbA1c and lipid profile testing if not assessed within the past year. Hormonal evaluation should include early-morning fasting total testosterone, with free or bioavailable testosterone measured when needed. Additional tests such as PSA, prolactin, or LH may be considered in selected patients. Although these evaluations may not always identify the exact cause of ED, they help detect underlying comorbid conditions.
Minimal diagnostic evaluation (basic work-up) in patients with ED
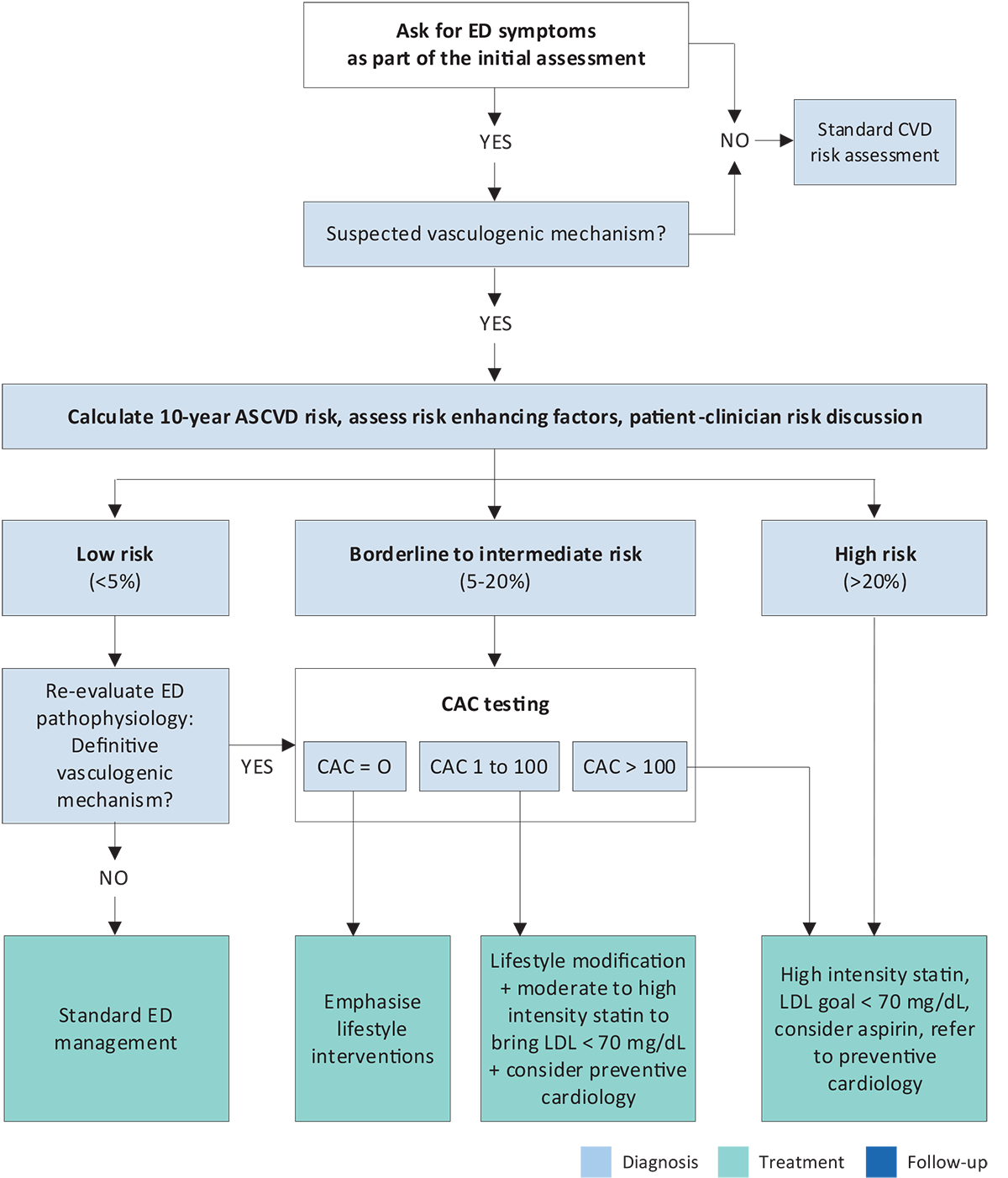
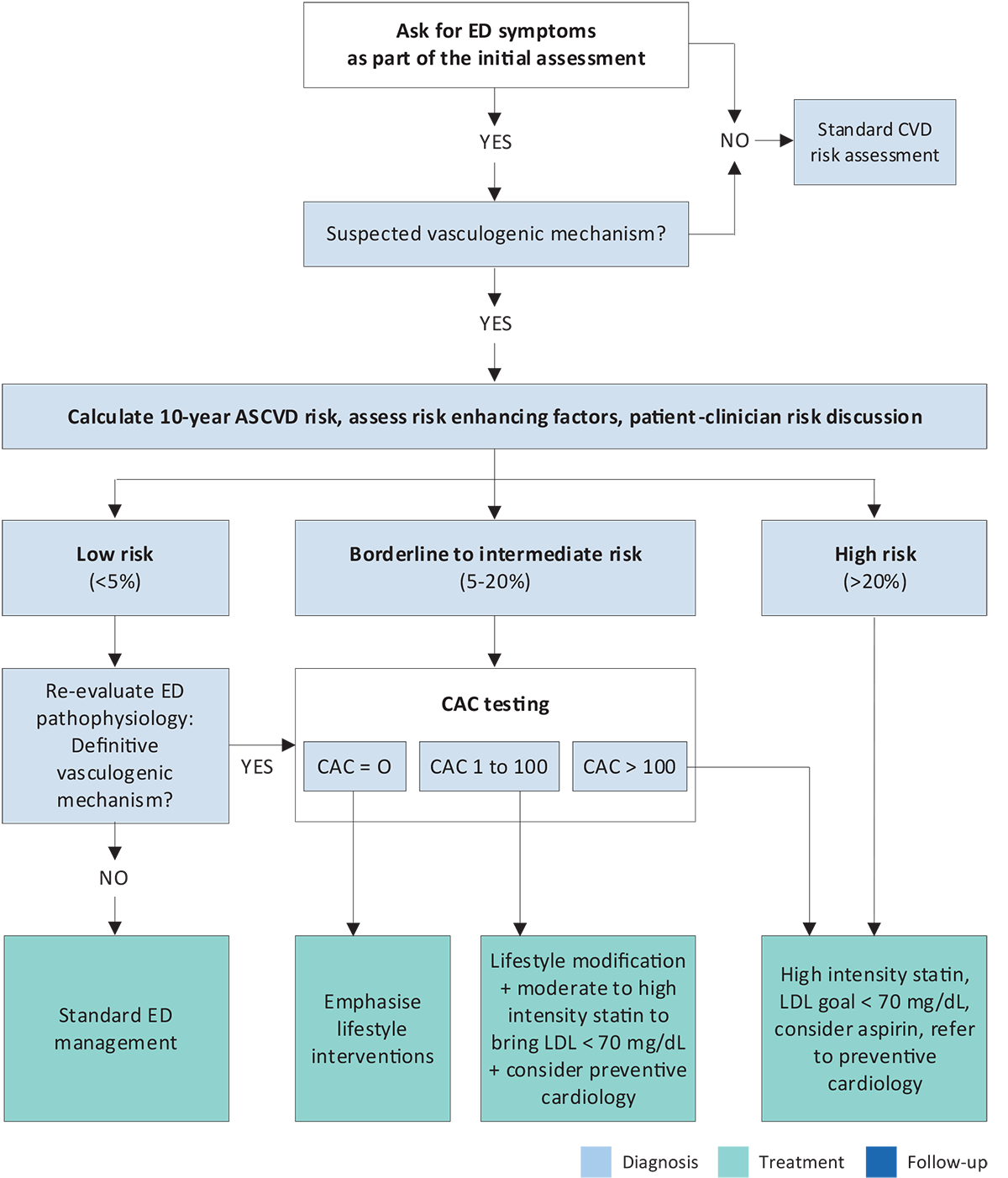
Cardiovascular system and sexual activity: the patient at risk
Patients presenting with erectile dysfunction have a high prevalence of cardiovascular disease, and ED is now recognized as an early marker and predictor of future cardiovascular events. The risk is particularly significant in younger men and increases with the severity and duration of ED. Therefore, ED should be considered a precursor of cardiovascular disease and an opportunity for early cardiovascular risk detection.
Current recommendations emphasize cardiovascular risk assessment in men with vasculogenic ED using the 10-year ASCVD risk score. In men with borderline to intermediate risk, coronary artery calcium scoring is advised to better detect subclinical coronary artery disease. These tools help guide safe sexual activity, treatment decisions, and overall cardiovascular risk management, while considering individual patient profiles, local expertise, and resource availability.
Cardiovascular system and sexual activity: the patient at risk
Management of ED in men with overt CV symptoms and/or CVD (based on IV Princeton Consensus)
Cardiovascular Risk Categories in Men With ED
Low-risk patients: Sexual activity poses minimal cardiac risk. These patients can perform moderate physical activity without symptoms and include those with well-controlled hypertension, successfully treated coronary disease, mild valvular disease, or stable heart failure (NYHA I–II).
Intermediate-risk patients: Patients with stable angina, recent myocardial infarction, moderate heart failure (NYHA III), or other atherosclerotic conditions such as stroke or peripheral arterial disease. Further cardiovascular evaluation, including stress testing or imaging, is required before resuming sexual activity.
High-risk patients: Patients with unstable or severe cardiac conditions where sexual activity is unsafe. This includes unstable angina, uncontrolled hypertension, severe heart failure (NYHA IV), very recent myocardial infarction, or high-risk arrhythmias. Sexual activity and ED treatment should be deferred until cardiac stabilization.
Diagnostic Evaluation (advanced work-up)
Most patients with erectile dysfunction can be managed based on their medical and sexual history, while some may require additional diagnostic testing.
Nocturnal penile tumescence and rigidity test
Nocturnal penile tumescence and rigidity (NPTR) testing uses overnight monitoring to assess the frequency, duration, and rigidity of nocturnal erections. The test should be performed on at least two nights, with normal erectile function indicated by rigidity of at least 60% lasting 10 minutes or more.
NPTR helps differentiate organic from psychogenic erectile dysfunction, as men with psychogenic ED usually show normal nocturnal erections. However, limitations and confounding factors restrict its routine use in clinical practice.
Intracavernous injection test
The intracavernous injection test provides limited information on vascular status. A positive result is a rigid erection within 10 minutes that lasts at least 30 minutes. However, the test alone is inconclusive, and penile duplex Doppler ultrasound should be performed if clinically indicated.
Dynamic duplex ultrasound of the penis
Dynamic penile duplex ultrasound is a second-level test used to assess haemodynamic causes of erectile dysfunction, particularly when vasculogenic ED is suspected. Normal findings include peak systolic velocity > 30 cm/s, end-diastolic velocity < 3 cm/s, and resistance index > 0.8. It may help tailor treatments such as low-intensity shock wave therapy. Further vascular testing is unnecessary if results are normal. However, its accuracy is limited by lack of standardisation and false positives, and its added value over the intracavernous injection test remains unclear. Accuracy can be improved with sexual stimulation or higher doses or combinations of vasoactive agents.
Arteriography and dynamic infusion cavernosometry or cavernosography
Pudendal arteriography should be performed only in patients being considered for penile revascularisation. Dynamic infusion cavernosometry and cavernosography are now rarely used for assessing venogenic erectile dysfunction, and the concept itself has been questioned. Computed tomography cavernosography is an emerging modality that provides detailed anatomical information to aid diagnosis and treatment planning.
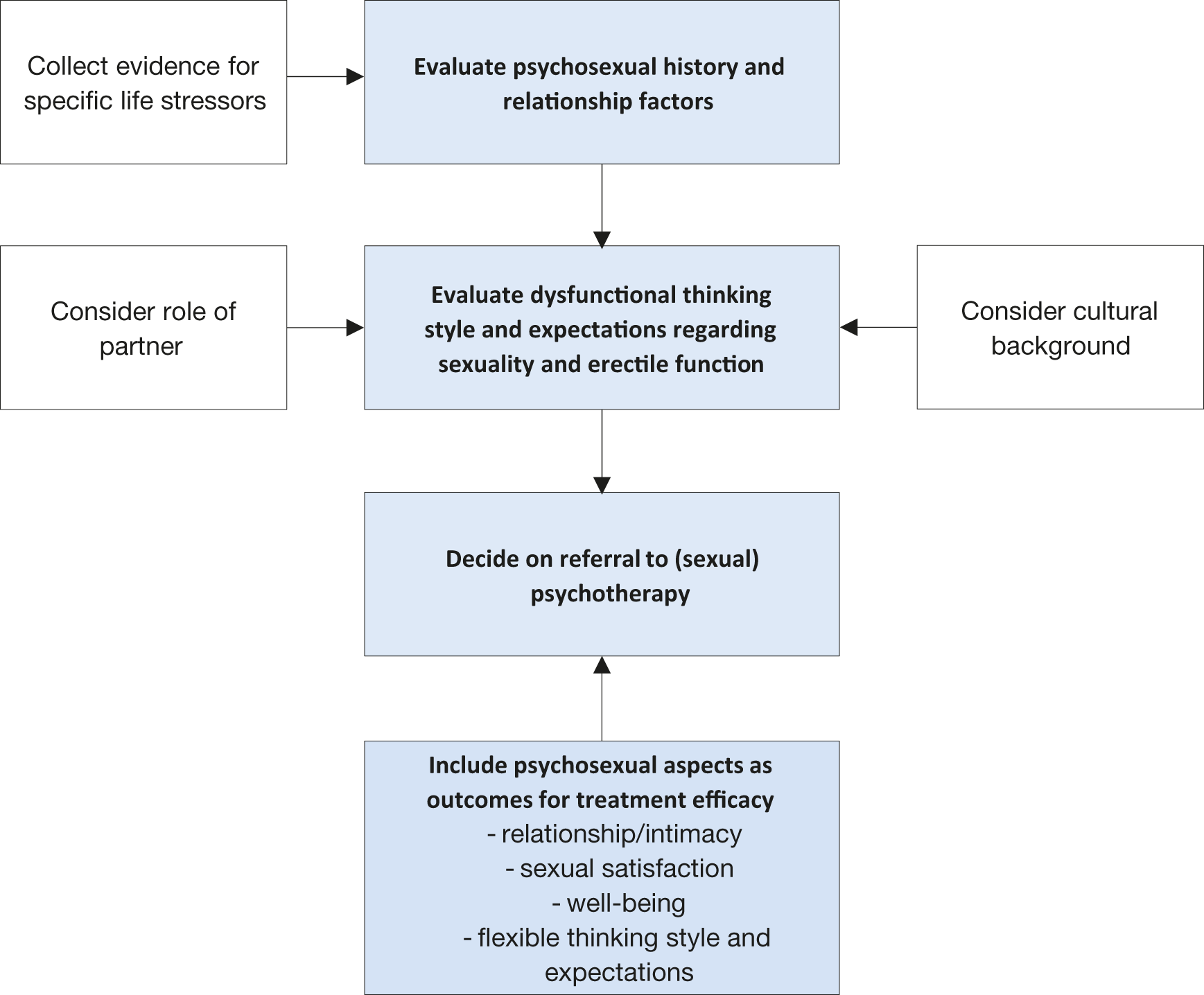
Psychopathological and psychosocial assessment
Mental health conditions, particularly depression and anxiety, as well as stress-related mood changes, are commonly associated with erectile dysfunction. Relationship difficulties and emotional disconnection can contribute to ED, while intimacy is protective. Cognitive factors such as negative sexual beliefs, low self-esteem, and distraction should also be evaluated. Psychosexual assessment includes a focused clinical interview and self-reported measures, and should be tailored for sexual minorities, as men who have sex with men may present specific psychological factors affecting erectile function.
Indications for specific diagnostic tests for ED and the specific diagnostic tests
Indications for Specific Diagnostic Tests in Erectile Dysfunction
| Indication | Description |
|---|---|
| Primary ED | Not due to acquired organic or psychogenic causes |
| Young patients with trauma | Pelvic or perineal injury; candidates for revascularisation |
| Penile deformities | Conditions requiring surgical correction |
| Psychosexual disorders | Complex psychiatric or psychosexual conditions |
| Endocrine disorders | Complex hormonal abnormalities |
| Patient/partner request | Assessment requested for reassurance or clarification |
| Medico-legal reasons | Documentation for end-stage ED or legal purposes |
Specific Diagnostic Tests for Erectile Dysfunction
| Category | Diagnostic Test |
|---|---|
| Erectile function | Nocturnal Penile Tumescence & Rigidity (Rigiscan®) |
| Vascular studies | Intracavernous vasoactive drug injection |
| Penile dynamic duplex ultrasonography | |
| Dynamic infusion cavernosometry & cavernosography | |
| Internal pudendal arteriography | |
| — | |
| Hormonal assessment | Specialised endocrinological studies |
| Psychosexual assessment | Specialised psycho-diagnostic evaluation |
Summary of evidence and recommendations for diagnostic evaluation of ED
| Summary of Evidence | LE |
|---|---|
| Medical and sexual history, physical examination, and laboratory testing including metabolic and hormonal profiles may identify risk factors and help define the aetiology of ED. | 3 |
| Validated psychometric questionnaires (e.g., IIEF, EHS) are reliable tools for assessing ED severity. | 3 |
| Specific diagnostic tests may help differentiate vasculogenic, hormonal, and psychogenic causes of ED. | 3 |
| Recommendation | Strength Rating |
|---|---|
| Take a comprehensive medical and sexual history in all patients with ED, including a targeted psychosexual assessment covering life stressors, cultural factors, and cognitive aspects of sexual performance. | Strong |
| Use validated ED-specific questionnaires (e.g., International Index of Erectile Function) to assess sexual function and treatment outcomes. | Strong |
| Perform a focused physical examination to identify underlying medical conditions and genital comorbidities associated with ED. | Strong |
| Evaluate laboratory tests, including glucose, lipid profile, and total testosterone, to detect reversible and modifiable risk factors. | Strong |
| Include specific diagnostic tests in the initial evaluation of ED when indicated by relevant clinical conditions. | Strong |
Treatment of erectile dysfunction
The Guidelines Panel has developed a comprehensive, personalised treatment algorithm for erectile dysfunction that moves beyond the traditional three-tier approach. Treatment is tailored to individual patients based on invasiveness, tolerability, effectiveness, and patient expectations, with full counselling on all available options. As most men do not receive cause-specific therapy, management relies on shared decision-making that considers efficacy, safety, cost, and patient preference. Ongoing physician–patient dialogue is essential, as treatment discontinuation is common and often influenced by beliefs about effectiveness, side effects, relationship factors, and cost.
Management algorithm for erectile dysfunction
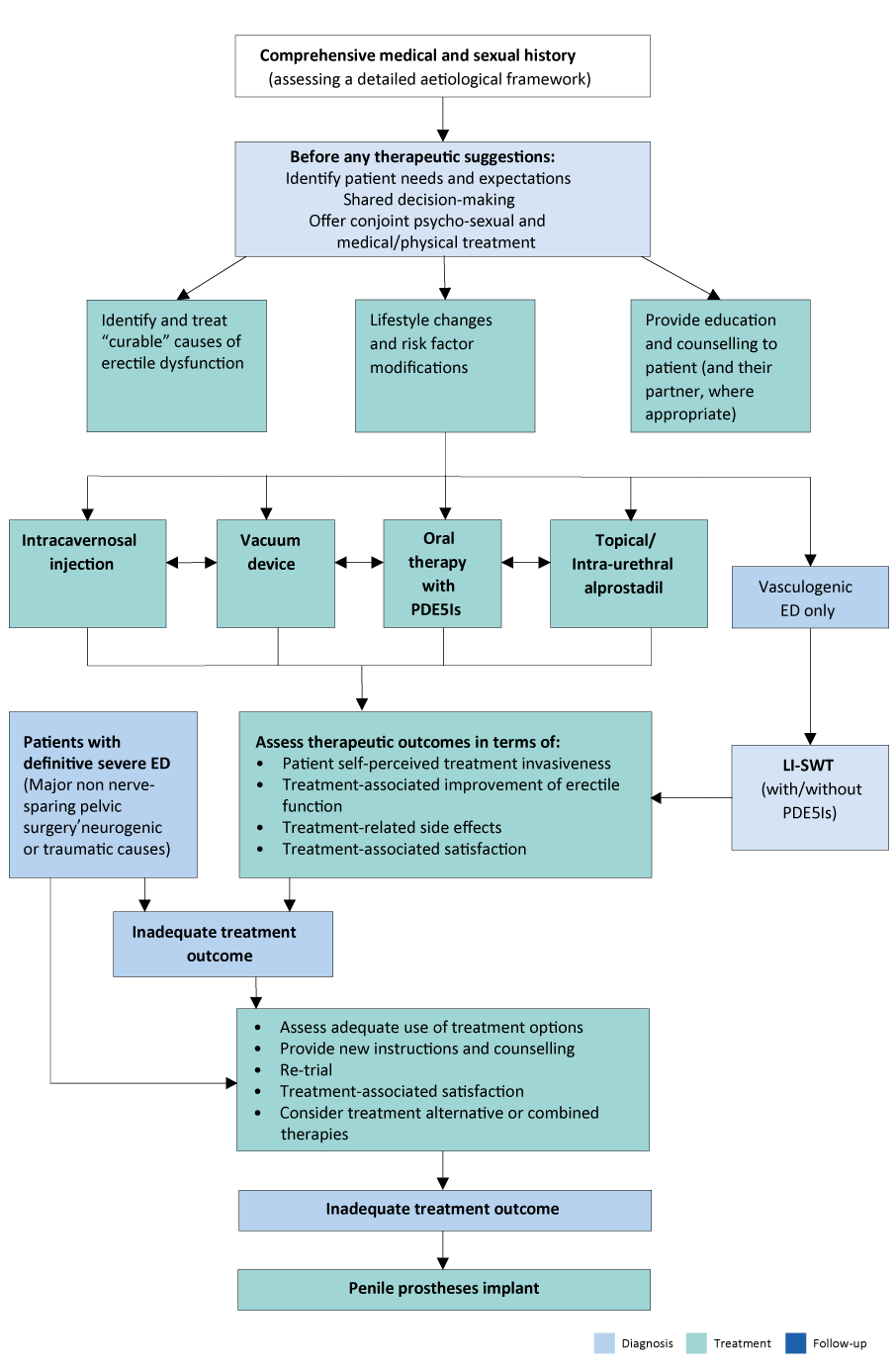
Patient education
Educational intervention is often the first step in managing sexual complaints and involves explaining the psychological and physiological aspects of sexual response in an understandable way. This approach can improve sexual satisfaction in men with ED. Patient consultations should address expectations and needs of both the patient and partner, review understanding of ED and diagnostic findings, and explain the rationale for treatment selection.
Modifiable risk factors
Erectile dysfunction is often associated with modifiable or reversible risk factors, including lifestyle habits and medication use, which can be addressed before or alongside specific therapies. ED is also commonly linked to underlying conditions such as endocrine, metabolic (e.g., diabetes), and cardiovascular disorders (e.g., hypertension), which should be optimally controlled as a first step in management. Evidence suggests that lifestyle modifications—particularly aerobic exercise, weight loss, and management of cardiovascular risk factors—can improve erectile function. The effect of statins on ED remains variable, with mixed evidence regarding benefit.
Phosphodiesterase type 5 inhibitors
Four selective PDE5 inhibitors are approved for the treatment of erectile dysfunction and have demonstrated efficacy across most patient subgroups. Efficacy is defined as achieving sufficient erectile rigidity for satisfactory intercourse, and adverse events are generally mild and self-limiting. The choice of PDE5 inhibitor depends on intercourse frequency and patient preference. Evidence suggests sildenafil may be preferred when maximising efficacy, while tadalafil may be favoured for better tolerability. Placebo responses are notable and may contribute to improved outcomes, particularly in men with ED associated with post-traumatic stress.
Sildenafil
Sildenafil is available in doses of 25, 50, and 100 mg, with a recommended starting dose of 50 mg that can be adjusted based on efficacy and tolerability. Its onset of action is typically 30–60 minutes, with effectiveness lasting up to 12 hours. Higher doses are associated with greater improvement in erectile function and patient-reported outcomes. Alternative formulations, including orally disintegrating tablets and oral suspension, are available for patients who have difficulty swallowing tablets.
Tadalafil
Tadalafil is used either on demand (10 or 20 mg) or as a once-daily dose of 5 mg, with 10 mg recommended as the initial on-demand dose and adjusted based on response and tolerability. Its onset of action begins within 30 minutes, with peak effect around 2 hours and a duration of up to 36 hours. Tadalafil improves erectile function and has additional benefits on ejaculatory and orgasmic function. Daily tadalafil 5 mg is also effective in men with erectile dysfunction and concomitant lower urinary tract symptoms due to benign prostatic hyperplasia, making it a suitable single-therapy option for both conditions.
Vardenafil
Vardenafil is administered on demand at doses of 5, 10, or 20 mg, with 10 mg recommended as the starting dose and adjusted based on response and tolerability. It is effective from about 30 minutes after intake, with some patients responding as early as 15 minutes. Vardenafil improves erectile function and patient-reported outcomes, including sexual performance and treatment satisfaction. An orodispersible tablet formulation is available, with efficacy comparable to the conventional tablet.
Avanafil
Avanafil is used on demand at doses of 50, 100, or 200 mg, with 100 mg recommended as the starting dose taken 15–30 minutes before sexual activity and adjusted based on efficacy and tolerability. It improves successful intercourse rates compared with placebo and has efficacy comparable to other PDE5 inhibitors, including sildenafil, vardenafil, and tadalafil.
Continuous use of PDE5Is
A once-daily tadalafil regimen (2.5 or 5 mg) may be considered based on patient preference and clinical judgement, with 5 mg taken at the same time each day as the recommended dose. Daily tadalafil offers greater spontaneity for couples and is suitable for those anticipating frequent sexual activity. Clinical outcomes are comparable between daily and on-demand tadalafil, and the daily regimen is generally well tolerated and effective across ED severities, including in partial responders to on-demand therapy. The need for continuous daily use should be reassessed periodically.
Pharmacokinetics data for PDE5Is EMA approved for the treatment of EDs
| Parameter | Sildenafil (100 mg) | Tadalafil (20 mg) | Vardenafil (20 mg) | Avanafil (200 mg) |
|---|---|---|---|---|
| Cmax | 560 μg/L | 378 μg/L | 18.7 μg/L | 5.2 μg/L |
| Tmax (median) | 0.8–1 h | 2 h | 0.9 h | 0.5–0.75 h |
| Half-life (T½) | 2.6–3.7 h | 17.5 h | 3.9 h | 6–17 h |
| AUC | 1,685 μg·h/L | 8,066 μg·h/L | 56.8 μg·h/L | 11.6 μg·h/L |
| Protein binding | 96% | 94% | 94% | 99% |
| Bioavailability | 41% | NA | 15% | 8–10% |
Adverse Events of PDE5 Inhibitors
| Adverse Event | Sildenafil | Tadalafil | Vardenafil | Avanafil (200 mg) |
|---|---|---|---|---|
| Headache | 12.8% | 14.5% | 16% | 9.3% |
| Flushing | 10.4% | 4.1% | 12% | 3.7% |
| Dyspepsia | 4.6% | 12.3% | 4% | Uncommon |
| Nasal congestion | 1.1% | 4.3% | 10% | 1.9% |
| Dizziness | 1.2% | 2.3% | 2% | 0.6% |
| Abnormal vision | 1.9% | — | < 2% | None |
| Back pain | — | 6.5% | — | < 2% |
| Myalgia | — | 5.7% | — | < 2% |
Safety concerns for PDE5Is
Cardiovascular safety: Available evidence shows no increased risk of myocardial infarction in patients treated with PDE5 inhibitors. In men with stable coronary artery disease, PDE5 inhibitor use has been associated with lower risks of mortality and cardiovascular events compared with alternative therapies. PDE5 inhibitors do not adversely affect exercise capacity or time to ischaemia in patients with stable angina. Current guidelines support the safe use of PDE5 inhibitors in patients with cardiovascular disease or high cardiovascular risk when prescribed appropriately.
Cardiovascular safety: Available evidence shows no increased risk of myocardial infarction with PDE5 inhibitors. In men with stable coronary artery disease, PDE5 inhibitor use is associated with lower cardiovascular event rates compared with alternative therapies. PDE5 inhibitors do not impair exercise tolerance or time to ischaemia in stable angina and are considered safe in patients with cardiovascular disease or high cardiovascular risk when appropriately prescribed.
Contraindications with nitrates and nicorandil: The concomitant use of PDE5 inhibitors with organic nitrates, nitric oxide donors (including recreational nitrites), or nicorandil is absolutely contraindicated due to the risk of severe hypotension caused by excessive cGMP accumulation.
Antihypertensive drugs: Co-administration of PDE5 inhibitors with antihypertensive agents may cause mild additive blood pressure reductions, which are usually clinically insignificant. The safety profile of PDE5 inhibitors is generally not worsened, even in patients receiving multiple antihypertensive medications.
Interactions with α-blockers: Tadalafil 5 mg is the only approved therapy for both erectile dysfunction and lower urinary tract symptoms and may be used alone or with α-blockers in men with mild-to-moderate symptoms. Although both drug classes are vasodilators, combined therapy does not significantly increase the risk of hypotension, and no current restrictions exist for their concurrent use.
Management of non- or poor-responders to PDE5 inhibitors: Management begins with confirming correct prescription, timing, dosing, and adequate sexual stimulation. High-fat meals may delay absorption of some PDE5 inhibitors. Patient education can restore response in many cases. In men with testosterone deficiency, testosterone therapy may improve PDE5 inhibitor efficacy. Switching between PDE5 inhibitors may benefit selected patients, although evidence is limited. In refractory cases, combination therapies may be considered.
Topical and intra-urethral alprostadil: Alprostadil may be administered topically at the urethral meatus or via intra-urethral pellets. Topical formulations improve erectile function in mild-to-severe ED with generally mild, transient local side effects. Intra-urethral alprostadil produces erections sufficient for intercourse in a subset of patients and is initiated at moderate doses, with titration as needed. Although less effective than intracavernous therapy, intra-urethral treatment offers a less invasive alternative for selected patients.
Psychosocial intervention and therapy
Psychosocial approaches, including sexual skills training, marital therapy, psychosexual education, and Cognitive Behavioural Therapy (CBT), are recommended in the management of erectile dysfunction. CBT, delivered individually, in couples or groups, and including online formats, targets dysfunctional cognitive and behavioural patterns and improves psychological adjustment. When combined with medical treatment, CBT is supported by evidence and is considered an optimal therapeutic approach.
Hormonal treatment
When clinically indicated, testosterone therapy may be considered in men with low or low-normal testosterone levels and associated symptoms such as reduced sexual desire, erectile dysfunction, and dissatisfaction with sexual activity. Testosterone can be administered via intramuscular, transdermal, or oral formulations and may be used in patients with cardiovascular disease following appropriate evaluation.
Vacuum erection devices
Vacuum erection devices are effective in achieving erections sufficient for intercourse across different causes of erectile dysfunction. Satisfaction varies and long-term adherence may decline. Common adverse effects include pain, bruising, numbness, and difficulty with ejaculation. Serious complications are rare with correct use. Vacuum devices are contraindicated in patients with bleeding disorders or those on anticoagulant therapy and may be suitable for patients seeking non-invasive, drug-free treatment.
Intracavernous injection therapy
Intracavernous injection of vasoactive agents is an established and effective treatment for erectile dysfunction and can be offered at any stage of a personalised treatment approach. Proper patient education is essential to ensure safe and effective use.
Alprostadil
Alprostadil is an established intracavernous treatment for erectile dysfunction, used as monotherapy at doses of 5–40 μg. Erection usually occurs within 5–15 minutes and is dose dependent. In-office training is required before use. High efficacy and satisfaction rates have been reported across different ED populations, including men with diabetes and cardiovascular disease. Common adverse effects include penile pain, prolonged erection, priapism, and fibrosis, which are generally mild or reversible. Systemic adverse effects are uncommon. Contraindications include hypersensitivity, bleeding disorders, and conditions predisposing to priapism. Despite good efficacy, discontinuation rates are high, underscoring the importance of proper counselling and follow-up.
Other vasoactive intracavernous treatments
Combination intracavernous therapy allows the use of lower drug doses while improving efficacy and reducing adverse effects. Papaverine and phentolamine are commonly used in combination due to limited efficacy or higher adverse effects when used alone and are not licensed as monotherapy for erectile dysfunction. Various other agents have been studied, but data are limited and availability is variable. Bimix and Trimix combinations are widely used and show high efficacy, with Trimix demonstrating the highest response rates, though fibrosis is more frequent when papaverine is included. A combination of vasoactive intestinal peptide and phentolamine has shown high effectiveness with a low risk of penile pain and priapism. Despite overall high efficacy, a small proportion of patients remain non-responsive to combination intracavernous therapy.
Intracavernous Injection Therapies
| Name | Substance | Dosage | Efficacy | Adverse Events | Comment |
|---|---|---|---|---|---|
| Caverject™ / Edex / Viridal™ | Alprostadil | 5–40 µg/mL | ~70% | Penile pain, priapism, fibrosis | Easily available |
| Papaverine | Papaverine | 20–80 mg | <55% | Elevated liver enzymes, priapism, fibrosis | Abandoned as monotherapy |
| Phentolamine | Phentolamine | 0.5 mg/mL | Poor as monotherapy | Systemic hypotension, reflex tachycardia, nasal congestion, GI upset | Abandoned as monotherapy |
| Bimix | Papaverine + Phentolamine |
Papaverine 30 mg/mL Phentolamine 0.5 mg/mL |
~90% | Similar to alprostadil (less pain) | Not licensed for ED |
| Trimix | Papaverine + Phentolamine + Alprostadil |
Papaverine 30 mg/mL Phentolamine 1 mg/mL Alprostadil 10 µg/mL |
~92% | Similar to alprostadil (less pain) | Not licensed for ED |
| Invicorp™ | VIP + Phentolamine | 25 µg + 1–2 mg | ~80% | Similar to alprostadil without pain | Easily available |
Innovative treatment modalities
Several novel treatment approaches for erectile dysfunction are currently under investigation. Most require further evaluation in large, well-designed, placebo-controlled randomised studies before evidence-based and clinically reliable recommendations can be made.
Regenerative medicine therapies
Shockwave therapy: Low-intensity shockwave therapy (LI-SWT) has been proposed as a treatment for vasculogenic erectile dysfunction and is the only marketed option with potential restorative effects. Clinical studies suggest improvement in erectile function, particularly in men with mild vasculogenic ED, although outcomes vary due to differences in devices, energy settings, and treatment protocols.
Overall benefits appear modest, with satisfactory improvement reported in a proportion of patients. Evidence suggests possible benefit in selected men with moderate to severe ED, including poor or non-responders to PDE5 inhibitors, and when combined with other treatments. Treatment effects usually appear within a few months and may decline over time. Current evidence remains limited and heterogeneous, and further high-quality studies are required before firm clinical recommendations can be made.
Platelet-Rich Plasma: Intracavernous platelet-rich plasma (PRP) injections have been investigated as a regenerative treatment for erectile dysfunction, based on the release of growth factors that may promote angiogenesis and tissue repair. Clinical studies have reported improvements in erectile function scores in men with mild to moderate vasculogenic ED, with a generally favourable safety profile.
However, study results are heterogeneous, with some trials showing benefit and others demonstrating no significant difference compared to placebo. Variability in preparation methods, dosing, activation protocols, and outcome measures limits interpretation. Although meta-analyses suggest modest improvement in erectile function, current evidence is insufficient to support routine clinical use. PRP therapy for ED should therefore be limited to clinical trial settings until larger, well-designed studies establish its efficacy and safety.
Stem-cells: Stem-cell therapy is being investigated as a regenerative treatment for erectile dysfunction. Early-phase clinical trials suggest that intracavernous stem-cell injections are generally safe; however, evidence of efficacy remains inconclusive due to small study sizes, heterogeneous protocols, and limited placebo-controlled data. At present, available evidence is insufficient to support clinical use outside of research settings.
Botulinum neurotoxin
:Botulinum neurotoxin A (BoNT-A) has been investigated as a treatment for erectile dysfunction in patients unresponsive to PDE5 inhibitors or intracavernous therapies. Randomised studies suggest improvements in erectile rigidity and sexual function, with some patients regaining satisfactory sexual activity. Adverse effects are generally mild and local, with no significant systemic complications. However, current evidence is insufficient to recommend routine clinical use, and larger controlled trials are required to confirm efficacy and safety.
Herbal medicine and natural supplements
The use of herbal medicines and natural supplements for erectile dysfunction has increased substantially, but robust scientific evidence supporting their efficacy and safety is limited. Available studies suggest that agents such as ginseng, L-arginine, and other antioxidants may produce small improvements in erectile function, which are often not clinically meaningful or perceived by patients. Combination therapy with PDE5 inhibitors and antioxidants may offer modest additional benefit. Overall, current evidence is insufficient to recommend herbal or antioxidant supplements as standard treatment for erectile dysfunction, and further high-quality studies are required.
Erectile Dysfunction After Radical Prostatectomy
Urologists should actively address erectile dysfunction (ED) after radical prostatectomy (RP) and offer treatment early. Early intervention may support recovery of erectile function (EF), although evidence for an optimal penile rehabilitation strategy remains limited. Phosphodiesterase type 5 inhibitors (PDE5Is) are the first-line treatment after nerve-sparing RP. Outcomes depend on patient age, baseline EF, and surgical technique, with mixed evidence regarding the benefit of daily versus on-demand use.
For patients unresponsive to oral therapy, intracavernosal injections, vacuum erection devices (VEDs), and penile implants are effective alternatives. Combination therapy with PDE5Is and VEDs may provide better results.
Adjunct options such as penile traction devices and pelvic floor muscle training show potential benefits, but further high-quality studies are required.
Surgical management
Surgery for post-traumatic arteriogenic ED
In young men with erectile dysfunction following pelvic or perineal trauma, penile revascularisation surgery can achieve long-term success rates of approximately 60–70%. Arterial stenosis must be confirmed using penile pharmaco-arteriography, and corporeal veno-occlusive dysfunction should be excluded with dynamic infusion cavernosometry or cavernosography.
Venous ligation surgery
Venous ligation surgery for veno-occlusive dysfunction is no longer recommended due to poor long-term outcomes.
Penile Prostheses:
Penile prosthesis implantation is indicated in men with erectile dysfunction who are unsuitable for, prefer to avoid, or do not respond to pharmacological or less invasive treatments. Available devices include inflatable (two- and three-piece) and semi-rigid prostheses, with no evidence demonstrating superiority of one type over another. Three-piece inflatable implants are often preferred for more natural erections, while two-piece and semi-rigid devices may be suitable in selected patients, including those with prior abdominal surgery or limited manual dexterity.
Implantation can be performed via penoscrotal or infrapubic approaches, with no clear advantage of either technique. With appropriate counselling, penile prostheses achieve very high satisfaction rates for both patients and partners, making them a definitive and effective treatment option.
The main complications are mechanical failure and infection. Modern inflatable devices show low mechanical failure rates and good long-term durability. Infection rates are low with meticulous surgical technique, antibiotic prophylaxis, coated implants, and strict infection-prevention protocols. Risk factors for infection include diabetes, hypogonadism, spinal cord injury, and poor patient selection.
Prosthetic infection usually requires device removal, though immediate salvage and replacement may be successful in selected cases. Other rare complications include implant erosion, reservoir-related injuries, and glans ischaemia, particularly in patients with significant vascular disease.
Summary of evidence and recommendations for treatment of ED
| Recommendation | Strength Rating |
|---|---|
| Fully inform patients about the mechanism of action and correct use of PDE5 inhibitors, as incorrect use is a common cause of treatment failure. | Strong |
| Refer patients for cognitive behavioural therapy, including partner involvement when appropriate, combined with medical treatment to optimise outcomes. | Strong |
| Discuss with patients undergoing active prostate cancer treatment the risk of sexual changes beyond ED, including reduced libido, orgasmic changes, anejaculation, Peyronie’s-like disease, and penile size changes. | Strong |
| Initiate lifestyle modification and risk factor control before or alongside ED treatment. | Strong |
| Use PDE5 inhibitors as first-line therapy for erectile dysfunction. | Strong |
| Use intracavernous injections as an alternative first-line option in well-informed patients or as second-line therapy. | Strong |
| Use topical or intra-urethral alprostadil as an alternative first-line therapy in well-informed patients who are unsuitable for oral therapy, decline injections, or prefer a less-invasive option. | Weak |
| Use low-intensity shockwave therapy (LI-SWT), with or without PDE5 inhibitors, in patients with mild vasculogenic ED, those unsuitable for oral therapy, or poor responders to PDE5 inhibitors. | Weak |
| Use vacuum erection devices in well-informed patients seeking non-invasive, drug-free ED management. | Weak |
| Consider daily supplements containing L-arginine or ginseng in men with mild ED who decline pharmacological treatment, after counselling about the modest expected benefit. | Weak |
| Implant a penile prosthesis when other treatments fail or based on patient preference, ensuring full counselling on benefits and risks. | Strong |
| Inform patients that current evidence does not support any specific penile rehabilitation regimen. | Weak |
| Initiate pro-erectile treatments as early as possible after radical prostatectomy, pelvic surgery, or other curative prostate cancer treatments. | Weak |